Top 10 Evidence Based Foot Drop Strategies
Amy Bean
Wednesday, October 29th, 2025
#dropfoot#electricalstimulation#footdrop#nmesAFOMirror TherapyStroke rehabilitation
We’ve put together a practical reference guide for you featuring 10 recommended strategies to help manage and rehabilitate foot drop. These approaches are backed by current research and international clinical guidelines, ensuring they reflect best practices in neurological and physical rehabilitation.
Since foot drop can result from a variety of underlying causes, not every strategy may apply to every individual. However, we hope this guide serves as a valuable resource, offering a range of options to support your recovery journey and help you choose the methods that best suit your needs.
1. Orthotic
What are these?
Often called an AFO or Ankle Foot Orthosis, these are splints that are worn to help lift the foot when walking. They can either be custom made or off the shelf.
Custom made orthotics are typically for those that need a lot of support due to severe spasticity, unstable ankle, or loss of range of calf muscle preventing the foot going flat on the floor. An orthotist would assess and make a custom made splint which may require adjustments over time.
Top 10 Evidence Based Arm Recovery Strategies After Stroke With Saebo
Amy Bean
Wednesday, August 20th, 2025
Arm RehabilitationEvidence-based therapyNeurorehabilitationOccupational therapyPhysical therapyPhysiotherapySaebo toolsStroke careStroke RecoveryUpper limb exercises
This handy user guide of the Top 10 interventions for Stroke rehabilitation are supported by the latest UK and Ireland National Clinical Guidelines for Stroke, the Australian and New Zealand Stroke guidelines and Canadian Stroke Recommendations for Best Practice. A full reference can be found at the bottom of this post.
All dosage recommendations (“How much/How often”) comes from the best evidence available. For some interventions this is very concrete e.g. NMES for shoulder subluxation, and for others such as Mirror Therapy we know it works but exact guidance on dosage is not as well known so we have provided the best summary information available.
1. Electrical Stimulation : “NMES” or “FES
What Is it ?
An electrical current stimulates nerve activity in a targeted muscle to ellicit a muscle contraction. This can help build strength, enhance motor recovery and enable task practice when weak or no movement. If the movement generated is used to help practice a task this would FES (Functional Electrical Stimulation) and if used in isolation with no task it is NMES (Neuromuscular Electrical Stimulation).
How NMES Can Help Relieve Arthritis Symptoms and Improve Mobility
Amy Bean
Tuesday, April 15th, 2025
Arthritis reliefArthritis supportChronic pain solutionsJoint pain managementNeuromuscular electrical stimulationNMES therapyNon-invasive arthritis treatmentSaebo rehabilitation
Arthritis is a musculoskeletal condition in which the body’s joints wear over time leading to pain, stiffness, reduced function and mobility. The severity of the condition varies person to person, and symptoms can be intermittent. With over 10 million people suffering from Osteoarthritis in the UK, or 1 in 6 people, there are many people having their every day life impacted by this condition.
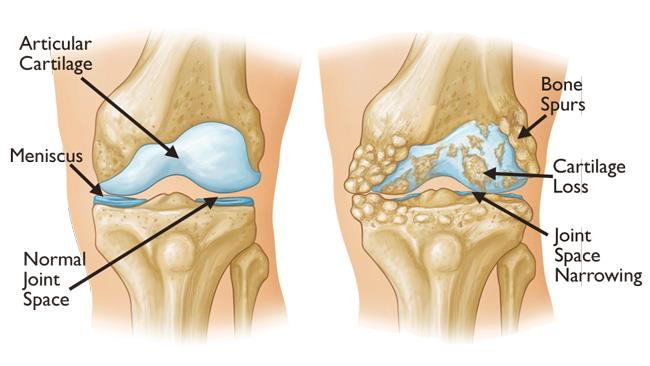
The most common joints affected are the knee, (approximately 5.4 million people), and the hip (approximately 3.2 million people).
Cartilage wears, joint space is reduced, and bony spurs develop on the joint surface , all leading to a joint that is painful to move and weight bear on.
Long term management can include surgery (e.g. joint replacements) and /or pharmaceutical management for pain. Non invasive management can include therapeutic exercise, education and weight loss where relevant, with the goal to improve pain and function for this long term, disabling condition.
Peripheral Nerve Injury
Amy Bean
Tuesday, August 13th, 2024
#dropfoot#electricalstimulation#footdrop#pain#painrelief#peripheralnerveinjury#TENS
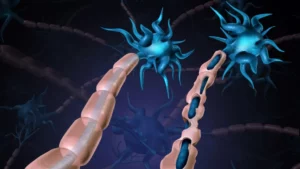
Our peripheral nervous system is a network of nerves that deliver motor, sensory and autonomic information (regulates body functions such as heart rate and digestion) from our brain and spinal cord to the rest of our body. Think of it like our telephone system sending messages and calls along telegraph lines to the end receiver and back again.
If any of the nerves are injured e.g. trauma, compression from bulging spinal disc, broken bones pushing on them etc., this disrupts the signals being sent. This can lead to weakness or absence of movement depending on the severity of the nerve damage, loss or altered sensation and for some people pain.
The injury can be partial meaning there is still some connection to send the electrical signals but movement is weaker, there is reduced sensation or altered pain; or it can be a complete severance of the nerve fibre resulting in no movement and sensation.
Treatment and management will be dependent on the extent of the nerve damage.
2024 : Celebrating 20 Years of Saebo UK and our SaeboFlex
Glyn Blakey
Monday, January 8th, 2024

Saebo UK and our SaeboFlex celebrate 20 years in the UK this year. This is our story of how it all started and the journey that the Saebo UK team have made…..
When we started in 2004, Constraint Induced Movement Therapy (CIMT) was the go to treatment for chronic stroke survivors, (i.e. at least 6 months post stroke). Saebo clinics were run based on the CIMT protocols with one to one supervision/assistance, but adapted for those unable to grasp and release by incorporating our SaeboFlex. The SaeboFlex was used for at least 3 hours a day, with the SaeboStretch as a night time resting splint and a session of electrical stimulation thrown in. After every SaeboFlex session, the stroke survivor was asked to attempt every day activities without the splint. This was 20 years ago and revolutionary at the time. Today, the literature is full of modified CIMT protocols to enable more people to follow this outside of the original very strict protocol.
TENS : Using Electrical stimulation for Pain Relief
Amy Bean
Tuesday, October 17th, 2023
#electricalstimulation#pain#painrelief#TENS
What is it?
Transcutaneous Electrical Nerve Stimulation, or TENS as it commonly referred to, is the use of electrical stimulation for pain relief.
In simple terms this type of electrical stimulation blocks the pain signals being sent to the brain and spinal cord to provide pain relief. It therefore doesn’t combat the cause of the problem but can provide much needed temporary relief for some users and is a potential alternative to medication.
Depending on the cause of the pain, the relief may provide relaxation to muscles that are in spasm because of the pain which will allow more freedom in movement. TENS can also stimulate the production of endorphins, our bodies natural pain killers.
Saebo Product Top Tips
Amy Bean
Monday, August 7th, 2023
At Saebo we strive to empower our customers with as much knowledge as possible to ensure our devices our used to their optimum.
To do this, in addition to the comprehensive manuals that come with each product, we have a number of different ways in which we provide additional product support.
Our Clinical Team, with over 45 years experience between them in Neurological Rehabilitation, are available to assist with any queries or support required. They can be contacted by email, phone, video calls, WhatsApp, and across our social media platforms.
Electrical Stimulation Contraindications: Facts and Myth Busting
Amy Bean
Tuesday, June 27th, 2023
#electricalstimulation#nmes#TENS

Before considering using neuro muscular electrical stimulation (NMES), users need to be aware of the contraindications and whether this treatment is safe to use.
A contraindication in medicine is a reason not to use something as it may cause harm.
It would be understandable to presume that there is an agreed set list of contraindications that apply internationally for everyone. Unfortunately this is not the case so in this blog we are going to go through the most commonly agreed contraindications in the UK and discuss each one. By having some knowledge of the reasons behind each one, and any research behind them, it will hopefully help more users to use this evidence based treatment as part of their rehab.
National Stroke Guidelines 2023
Amy Bean
Friday, April 14th, 2023
#strokerecovery#strokerehab#strokerehabilitation

On 4th April the new UK and Ireland National Stroke Guidelines 2023 were published. The last published guidelines were the 5th edition in 2016, and 7 years is a long time in medicine.
These Guidelines bring the biggest changes to Stroke Care and Rehabilitation that we have ever seen.
Almost 300 recommendations were reviewed and updated, 62 key questions searched, 676 papers reviewed and the Guidelines were drafted by a group of over 170 topic experts from the UK and ROI, and they are NICE (National Institute for Clinical Excellent) accredited.
Here at Saebo we have pored over the Guidelines and thought it would be helpful to highlight some key rehabilitation recommendations that stood out for us that are new to these Guidelines.
Sensory Electrical Stimulation for Pain Management
Amy Bean
Wednesday, March 1st, 2023
#electricalstimulation#pain#painrelief#TENS

The International Association for the Study of Pain defines pain as “An unpleasant sensory or emotional
experience associated with actual or potential tissue damage, or described in terms of such damage.” And this can be from many different causes ranging from arthritis in a joint, to muscle damage from a sports injury to “post stroke pain” which might be from a shoulder subluxation, spasticity or joint stiffness from lack of movement.
We have previously discussed the use of TENS for pain relief in a previous blog but in this blog we are going to go more in depth into the use of Sensory Electrical Stimulation to manage pain.
